Gynecomastia and pseudogynecomastia are two common conditions that cause enlarged breast tissue in men. While they may appear similar, there are key differences between gynecomastia and pseudogynecomastia. Understanding these differences is important for determining the right treatment approach.
This article will discuss how to differentiate between gynecomastia, how to know gynecomastia or pseudogynecomastia, their causes, symptoms, diagnosis, and treatment options.
What is Gynecomastia?
Gynecomastia is the enlargement of breast gland tissue in males. An imbalance between the hormones oestrogen and testosterone typically causes it. The condition can occur during developmental life stages like puberty or old age. Certain health conditions or medications may also bring it on.
True gynecomastia leads to extra glandular breast tissue. This tissue feels rubbery or firm and is located directly under the nipple and areola regions. Swelling occurs in a concentric pattern from the nipple.
What Causes Gynecomastia?
Some of the common causes of gynecomastia include:
Book A Consultation With Dr Tarek Bayazid
Top-rated Plastic Surgeon For Gynecomastia in Dubai
Installment Plan Available
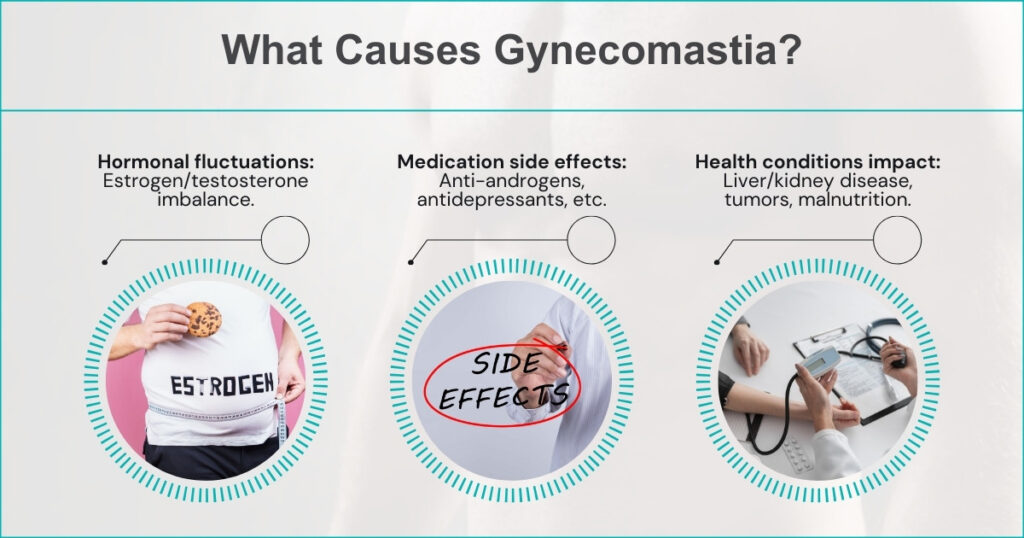
- Hormonal changes
Increased oestrogen levels and/or decreased testosterone levels can cause a hormonal imbalance leading to gynecomastia. This frequently occurs during puberty, old age or due to anabolic steroid use.
- Medications
Certain medications such as anti-androgens, calcium channel blockers, tricyclic antidepressants, anti-ulcer drugs and HIV treatments can cause gynecomastia as a side effect.
- Health conditions
Kidney or liver disease, underactive thyroid (hypothyroidism), cancerous tumours and malnutrition can all trigger gynecomastia by upsetting normal hormone balance.
Recognising Gynecomastia Signs
The main signs indicating gynecomastia rather than pseudogynecomastia include:
- Rubbery or firm breast tissue – The enlarged breast consists of real glandular tissue rather than just fat, so it feels rubbery/firm to the touch.
- Tissue under nipples/areolas – The subareolar region right beneath the nipple and areola is swollen with breast tissue.
- Bilateral development – Both breasts are symmetrically enlarged (though one side may be worse than the other).
- Nipple discharge – A clear or milky fluid may discharge from the nipple when squeezed.
- Breast tenderness/pain – Mild breast tenderness, sensitivity or a dull ache.
- Onset during developmental stages – Most commonly arises in infant boys, during adolescence and later stages of male ageing.
What is Pseudogynecomastia?
Pseudogynecomastia, or lipomastia, is fat tissue buildup rather than true breast gland tissue. It gives the appearance of gynecomastia but without the rubbery breast tissue swelling. This condition typically results from being overweight or obese. The fat often deposits in the chest region, giving the appearance of enlarged breasts.
Recognising Pseudogynecomastia Signs
The main indicators pointing to pseudogynecomastia rather than true gynecomastia are:
- Soft/fatty breast tissue – The enlarged area feels soft and fat-like rather than rubbery glandular tissue.
- Generalised chest enlargement – The full chest area appears swollen with fat rather than distinct tissue under the nipples.
- Uneven fat distribution – One breast may be larger than the other, with asymmetrical appearances.
- No nipple discharge – No fluid discharge from the nipples.
- No breast tenderness – The enlarged area is not usually painful or tender.
- Associated with obesity – Overall, high body fat is often centrally distributed on the chest.
How To Know Gynecomastia Or Pseudogynecomastia?

Some tests that can help differentiate gynecomastia from pseudogynecomastia include:
| Criteria | Gynecomastia | Pseudogynecomastia |
| Tissue Composition | Glandular breast tissue predominates | Excess fat without significant gland tissue |
| Palpation | Firm, rubbery mass under the nipple area | Soft, fatty feel more diffuse in the chest |
| Pain or Tenderness | Often tender or painful to touch | Usually, there is no pain or tenderness |
| Effect of Weight Loss | It may not significantly reduce weight loss | Reduces with overall body fat decrease |
| Age of Onset | Common in adolescents and older men | Typically overweight individuals |
| Response to Hormonal Changes | Affected by hormonal imbalances | Not influenced by hormonal changes |
This table compares the key aspects of diagnosing Gynecomastia and Pseudogynecomastia. It highlights the differences in tissue composition, sensation upon palpation, response to weight changes, age of onset, and reaction to hormonal fluctuations. This clear distinction aids in accurate diagnosis and appropriate treatment planning.
Diagnostic Tests
If the cause remains unclear based on a physical exam, there are a few tests that can confirm a diagnosis:
- Blood tests
These check hormone levels related to gynecomastia, like estradiol, testosterone, and human chorionic gonadotropin (hCG).
- Tissue biopsy
Removing a small sample of breast tissue for analysis can confirm excess glandular tissue typical of gynecomastia.
- Imaging
Mammograms or ultrasound imaging can help determine if the growth is caused by glandular breast tissue rather than fat alone.
Treatments for Gynecomastia and Pseudogynecomastia
The recommended treatment plans differ significantly between gynecomastia and pseudogynecomastia:
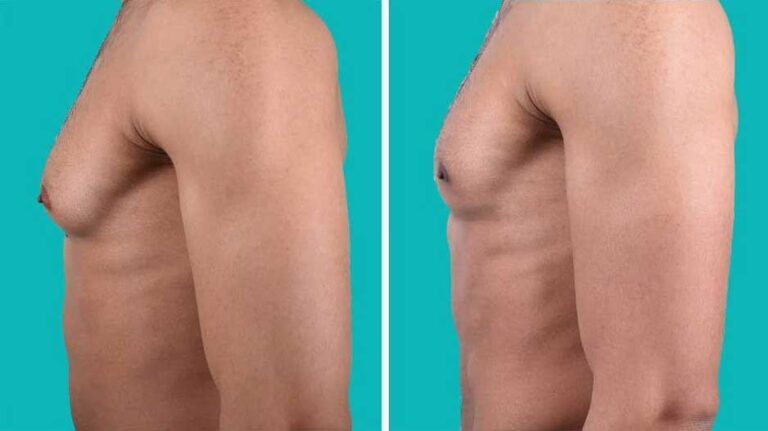
Gynecomastia Treatments
- Medication – Hormone-modulating medicines may help rebalance hormones and shrink breast tissue.
- Surgery – Either liposuction to remove breast fat or mastectomy to remove glandular tissue and skin.
Pseudogynecomastia Treatments
- Lifestyle changes – Diet, exercise, avoiding alcohol to promote weight and body fat loss overall.
- Liposuction – Removing excess chest fat can reduce the appearance of enlarged breasts.
As you can see, correctly understanding whether you have true gynecomastia or pseudogynecomastia is very important for determining the appropriate management and treatment. If you are unsure, consult a doctor or men’s health specialist for proper diagnosis and care recommendations tailored to your personal situation.
When to Seek Medical Care

You should see a doctor if you notice:
- Breast tissue growth
- Changes to the nipple
- Pain, tenderness, swelling, or discharge in one or both breasts
- Persistent symptoms for longer than 12 months after puberty
Early evaluation for gynecomastia or pseudogynecomastia can lead to faster relief of your symptoms.
Conclusion
Identifying the differences between glandular gynecomastia and pseudogynecomastia due to fat is key to getting the right treatment. For those wondering how to know gynecomastia or pseudogynecomastia, it’s essential to consult a doctor for a professional assessment. See your doctor if you notice any persistent breast changes to determine the appropriate next steps. With the right guidance, both gynecomastia and pseudogynecomastia can be effectively managed. Understanding gynecomastia how to know is the first step in seeking proper care and treatment.
Looking for professional guidance regarding gynecomastia or pseudogynecomastia?
If you’re questioning gynecomastia, booking a consultation with Dubai plastic surgeon Dr Tarek Bayazid is a crucial step. He will diagnose your specific case and chart out the ideal treatment plan. His expertise ensures accurate identification and effective management of your condition.
Dr. Tarek Bayazid, a distinguished plastic surgeon based in Dubai, specializes in facial rejuvenation, body sculpting, and gynecomastia surgery. His approach prioritizes patient care, blending modern techniques to deliver results that appear natural. With training from Europe and affiliations with respected societies, Dr. Bayazid is skilled in a range of procedures, from non-invasive treatments to intricate surgeries, all performed with a focus on safety and an artistic flair. Learn more about gynecomastia surgery cost in Dubai here.
FAQs about Gynecomastia and Pseudogynecomastia