Grade 1 gynecomastia guide covering symptoms, causes, medical treatment, surgery indications, and type 1 prognosis when enlargement is limited to the areolar region.
Gynecomastia type 1 treatment features slight breast enlargement confined to the areola. Hormonal changes often cause it, and it typically resolves on its own.
Treatment may not be needed unless the gynecomastia is painful, persistent, or impacting confidence. Initial options include reassurance, medications like tamoxifen, and weight loss.
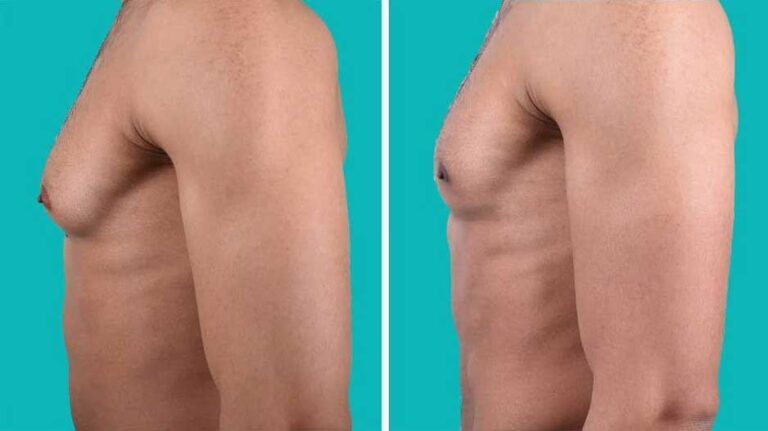
If distress continues despite conservative measures, subareolar tissue removal via a periareolar incision can be considered. This surgical approach effectively corrects type 1 gynecomastia.
What is gynecomastia type 1 Treatment?
Gynecomastia type 1 involves slight enlargement and protrusion limited to the areolar region.
Book A Consultation With Dr Tarek Bayazid
Top-rated Plastic Surgeon For Gynecomastia in Dubai
Installment Plan Available
- Characterised by the increased diameter of the areola
- Features only minor breast tissue proliferation
- Minimal distribution of fat in the breast area
- The nipple-areola complex remains above the inframammary fold
- Little to no skin redundancy or severe ptosis
- Asymmetry between two sides of the chest is common
What causes gynecomastia type 1?
Hormonal changes often cause gynecomastia type 1 during puberty or ageing, which leads to a temporary imbalance between estrogens and androgens.
- Pubertal hormone changes in adolescent boys
- Age-related decreases in testosterone
- Increased aromatase enzyme activity in older men
- Medications like spironolactone, cimetidine, etc.
- Endocrine disorders like hyperthyroidism
- Chronic illnesses such as liver disease or renal failure
- Idiopathic reasons with no identifiable cause
Should gynecomastia type 1 be treated?
Treatment for mild type 1 gynecomastia may not be necessary in many cases since the condition often resolves spontaneously, but it can be considered for persistent, painful, or emotionally distressing cases.
- Often resolves on its own in adolescents within 1-2 years
- Treatment is optional if it causes no physical symptoms or emotional distress
- Can consider treatment if persistent beyond 2 years
- Treatment indicated if pain, tenderness, or swelling is present
- Therapy is warranted if it significantly impacts self-esteem
- Treatment choices based on individual factors and preferences
What medications treat gynecomastia type 1?

For type 1 gynecomastia, medications like tamoxifen, raloxifene, and danazol may effectively reduce breast tissue proliferation and tenderness.
| Medication | Mechanism | Effectiveness | Side Effects |
| Tamoxifen | Estrogen receptor antagonist | Up to 80% response | Hot flashes, mood changes |
| Raloxifene | Estrogen receptor antagonist | Good short-term response | Leg cramps, blood clots |
| Danazol | Androgen effect | 60% response | Weight gain, muscle cramps |
| Anastrozole | Aromatase inhibitor | No proven added benefit | Bone/joint pain |
This table summarises the key medications used to treat gynecomastia type 1, how they work, typical response rates, and potential adverse effects. Tamoxifen and raloxifene are preferred first-line options.
When is surgery recommended for gynecomastia type 1?
Surgery is rarely indicated for mild type 1 cases but could be considered if other treatments fail or gynecomastia continues to cause psychological burden.
- Surgery is seldom required due to the mild degree of changes
- Primary option if persistent lump remains despite medication attempts
- Also, an option if gynecomastia severely affects self-confidence
- Usually delayed until after puberty if the adolescent case
- A combination of liposuction and adenectomy is not typically needed
- Adequate tissue removal is key to preventing the recurrence
See related: Gynecomastia cost in Dubai
What is the prognosis after surgery for gynecomastia type 1?
After surgery for gynecomastia type 1, outcomes are generally excellent, with low recurrence rates and high patient satisfaction when glandular tissue is adequately removed.
| Outcome | Rate | Factor Affecting |
| Recurrence | < 5% | Complete gland excision |
| Hypoesthesia | 50% | Nerve disruption, temporary |
| Hematoma | 10% | Drain use, compression |
| Reoperation | 5% | Residual lump |
| Satisfaction | 90% | Realistic expectations |
This table highlights the key prognostic outcomes following surgery for gynecomastia type 1, including common complications and high patient satisfaction rates.
Should gynecomastia type 1 be treated?
Treatment for mild type 1 gynecomastia may not be necessary in many cases since the condition often resolves spontaneously, but it can be considered for persistent, painful, or emotionally distressing cases.
- Often resolves on its own in adolescents within 1-2 years
- Treatment is optional if it causes no physical symptoms or emotional distress
- Can consider treatment if persistent beyond 2 years
- Treatment indicated if pain, tenderness, or swelling is present
- Therapy is warranted if it significantly impacts self-esteem
- Treatment choices based on individual factors and preferences
What lifestyle changes help gynecomastia type 1?
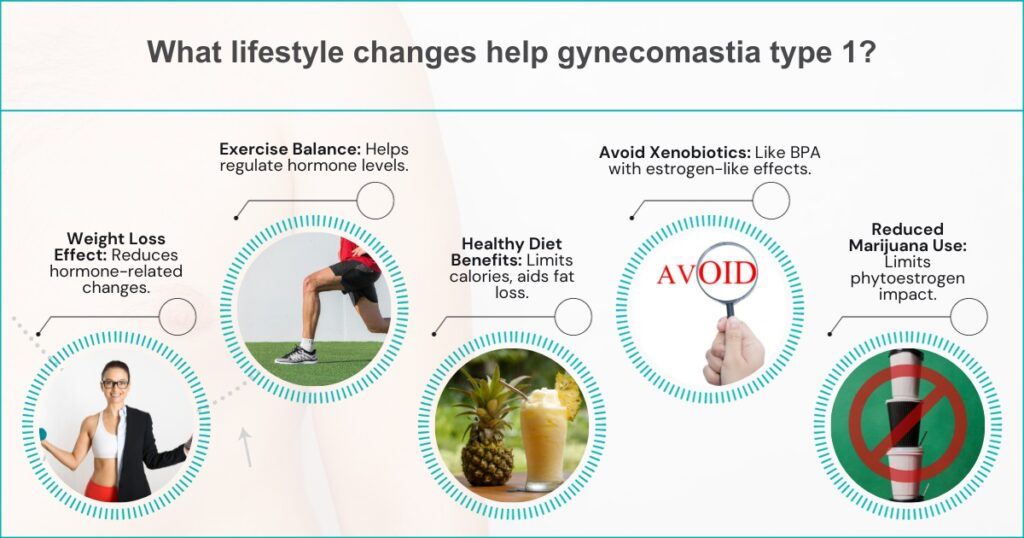
Lifestyle modifications like weight loss through diet and exercise can aid in resolving type 1 gynecomastia associated with hormone changes from obesity.
- Losing weight reduces aromatase enzyme activity.
- Regular exercise helps balance hormone levels
- A healthy diet limits calorie intake and promotes fat loss
- Avoiding xenobiotics like BPA that have estrogen-like effects
- Reducing marijuana use, which may act as a phytoestrogen
- Monitoring for recurrence if lifestyle regimen stopped
What is the prognosis for gynecomastia type 1?
The prognosis for mild type 1 gynecomastia is generally excellent, with most adolescent cases resolving within a couple of years without treatment.
- Favorable prognosis compared to more advanced grades
- Up to 95% of adolescent cases resolve spontaneously
- May persist beyond 2 years in 5% of teenage boys
- More likely to regress with age in adult-onset cases
- Does not typically progress to more severe grades
- Shallow risk of developing breast cancer
What surgical procedures treat gynecomastia type 1?

The standard surgery for gynecomastia type 1 is subareolar gland excision through a semicircular incision around the lower half of the areola.
| Approach | Details | Considerations |
| Incision | Periareolar semicircle | Cosmetic result |
| Gland excision | Subareolar tissue | Complete removal |
| Liposuction | Not indicated | Minimal fat |
| Drains | Closed suction | Prevent fluid accumulation |
| Revision | If recurrence | Re-excise residual tissue |
This outlines critical steps in the surgical procedure to treat grade 1 gynecomastia, focusing on complete subareolar gland excision through a periareolar incision with no need for liposuction or significant skin excisions.
Treatment for type 1 aims to address discomfort and burden when slight breast enlargement limited to the areola does not regress.
Dr Tarek is a leading Dubai plastic surgeon known for achieving natural-looking results. He takes a patient-focused approach and stays at the forefront of the latest techniques.
For expert gynecomastia treatment, consult renowned plastic surgeon Dr Tarek Bayazid. Book a consultation to discuss the options he recommends.
See related:- gyno surgery dubai cost